The Midwest Diabetes Conference, hosted by the Illinois Primary Health Care Association in collaboration with the Association of Diabetes Care and Education Specialists, offered insight into future trends of diabetes and evidence-based treatment approaches. One approach highlighted during the Self-Management portion was the Diabetes Prevention Program (DPP). This year-long program aims to identify those most at-risk and provides them with education and peer support. It also utilizes a lifestyle coach, physician, and group programs to create and maintain healthy habits.
Prediabetes – The Tipping Point to Type 2
According to the conference, 34.1 million American adults have diabetes. Within that demographic, only one in five people are aware of their diagnosis. Additionally, as the prevalence of diabetes increases with age, it is also highest among American Indians, Hispanic Americans, non-Hispanic Black Americans, and some Asian American and Pacific Islanders.
However, prevalence of prediabetes is similar across all racial and ethnic groups and is rising at an alarming rate. 88 million American adults, or one in three, have prediabetes. Despite this, eight in ten people with it are unaware of their diagnosis. Prediabetes, formerly called impaired glucose tolerance, is a serious condition where blood sugar levels are higher than normal but not yet severe enough to be diagnosed as diabetes. Because the condition precedes type 2 diabetes, early detection and intervention is encouraged to delay or prevent this progression.
Millions of Americans are currently at risk of developing type 2 diabetes by 2050 – a health crisis that would have a catastrophic effect on health care systems, patients, and the economy. Type 2 diabetes can lead to complications with and slower recoveries from surgeries. It can also cause comorbidities in other areas of physical, behavioral, and mental health.
However, people must first be aware of the problem in order to recognize possible solutions. Combatting the prevalence of prediabetes and slowing the rate of type 2 diabetes begins with identifying those most vulnerable and using a quadruple aim approach. This approach should strive to improve population health, reduce costs for patients and providers, support the wellbeing of the health care staff, and provide an excellent patient experience.
Diabetes Prevention Program Overview
The Diabetes Prevention Program (DPP), a pilot study from 1996-1999, combined one-on-one provider visits, peer support, and intensive lifestyle changes including medication if needed to intervene before prediabetes hits the tipping point into type 2. It also offered a flexible approach which allows care facilities to tailor the program to the specific expertise of their staff and the needs of the demographics and patients they serve.
The pilot study split patients with prediabetes, all of whom were overweight according to the BMI Scale, into three groups. One group was given a placebo with minor lifestyle change suggestions, such as eating healthier and increasing physical activity. The second group was given 850 mg of metformin twice daily to help prevent type 2 diabetes.
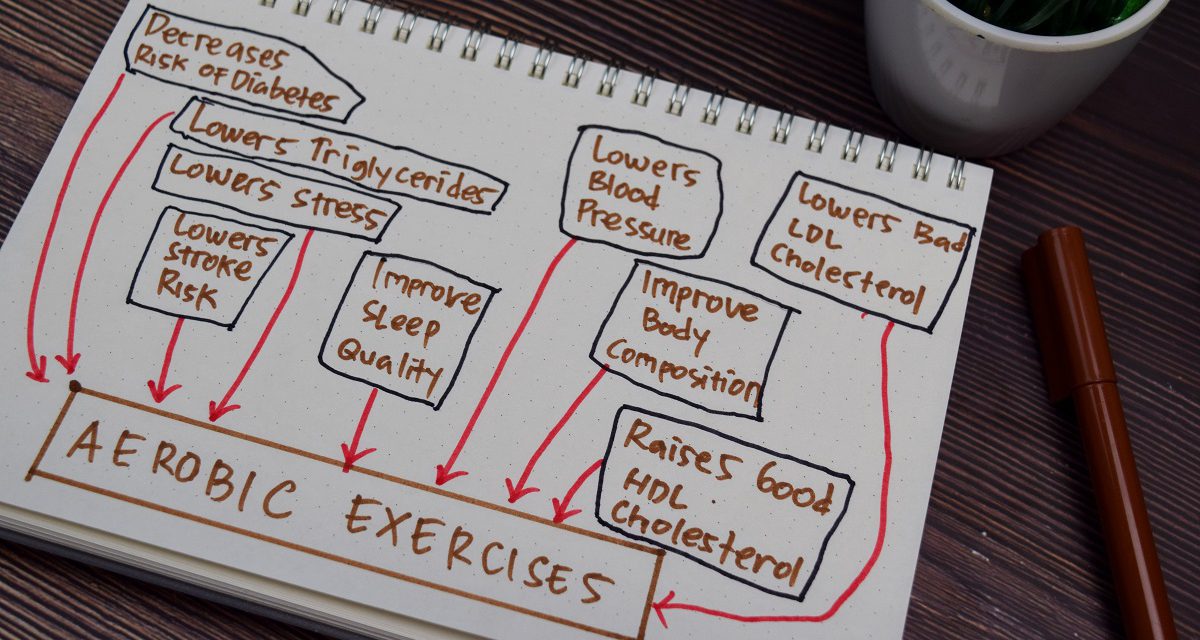
The third group underwent an intensive lifestyle modification including but not limited to goal-focused healthy eating, completing 150 minutes of physical activity per week, and losing a certain percentage of their BMI. Medication was still effective across certain demographics, but the lifestyle changes played the greatest role.
While the placebo group was largely ineffective, the combination of lifestyle changes and medications proved far more effective. The group solely taking metformin saw a 31% decrease in prediabetes over the program duration. Metformin was most effective in younger participants, those with the highest BMIs, and some women. The lifestyle support group, however, saw a 58% decrease. Participants over 60 years old in the lifestyle group saw a decrease of 71%.
Much of this success was credited to the group format. While the patients had brief individual physician visits to discuss medication or other needs, the majority of the program was offered through group meetings with a lifestyle coach. This format allowed patients navigating prediabetes and diabetes to support and validate each other, offer advice, and foster motivation and accountability. In Diabetes Prevention Programs today, these meetings can also be held via telehealth programs, allowing flexibility and reducing access barriers for those who cannot physically attend.
The coaches in these programs can also be flexible as they aren’t required to be a diabetes specialist. Because patients will already meet with a physician, the lifestyle coach can be employed from a provider’s existing staff based on their skills. The flexibility of the group setting, lifestyle coaches, and modalities in existing resources allow providers to implement the program for less than a third of its original cost.
Overall, the pilot study succeeded in all four areas of its quadruple aim approach. Current and future programs making the most of the flexibility can expect to see similar results.
- Population health: Participating patients not only reduce diabetic risks and prevalence in other aspects of their health but are also more likely to give referrals. As they encounter others with diabetes, they’ll speak to the program’s success and its long-term upkeep through the various other programs offered, bringing information about diabetes and the Diabetes Prevention Program into a new space.
- Cost reduction: Patients invested in their health are less likely to miss appointments or utilize emergency services. Additionally, taking preventive measures and engaging in other helpful facility programs continues to reduce their health risks.
- Care team wellbeing: Providers grow more confident as they see patients succeed. Learning about various experiences with diabetes in a group setting also provides them more lived-experience knowledge moving forward.
- Patient experience: Because patients have more face time with coaches than they usually do with physicians, they receive more direct support, can tangibly track and celebrate progress, and receive the support to continue outside of and after the program.
Implementing a Diabetes Prevention Program
Addressing the imminent type 2 diabetes crisis requires early identification, discussion, and treatment. Conference panelists recommend using prediabetes screenings for at-risk patients and having printed versions available in waiting areas. These screenings can help begin a conversation with the patient around the risks they face and their options to guide their treatment. The benefit to utilizing DPP is the investment patients take in their own health.
To implement these programs, experts recommend beginning with what you already have. Pre-existing programs focusing on healthier habits are a perfect gateway to discussing how the skills patients are already learning can be utilized to improve their health. While it may be difficult to persuade a patient to join an intensive 12-month program, helping someone participate in a healthy cooking class and put their new skills to use may be easier. Lunch and learn meetings, summer gardening and fitness classes, and monthly drop-in support groups are all excellent places to start.
Considering the emotional toll and stress of daily health observance and management for diabetic patients, coaches can also be a make-or-break factor for the program’s success. Instead of hiring a diabetes specialist or educational coach, utilize the existing team to their strengths. Coaches should be friendly, motivating, and able to encourage others to care about their health.
Providers who have found success with the program suggest choosing coaches who are culturally humble, flexible, intuitive, independent, passionate, consistent, and outgoing. Although the Diabetic Prevention Program encourages a team approach and weekly check-ins to assess patients’ progress and needs, coaches who can sufficiently balance the individual needs of the group are a priceless asset.
Success has also largely been found using incentives. Possible incentives that promote better health include scales, pedometers, exercise gear, food program supports, transportation vouchers, cooking utensils, and groceries. Incentivizing the group meetings, though not required, motivates patients to consistently attend and also offers opportunities for more collaborations.
One program offered fresh produce to attendees, helping them stock up on groceries more aligned with their new health goals. This collaboration not only benefited the program, but also boosted a local Black-owned farm and fostered community connections. Partnering with local agriculture to provide food creates opportunities for continued partnering, such as hosting a healthy recipe cooking class using fresh food from local farms.
Above all, participants have responded best to celebratory shoutouts on social media and certificates showing completion of the program at midpoint and graduation. The encouragement and support provided by a team of peers and coaches cheering them on has proven powerfully effective.
An Investment for Life
Helping patients invest in their health not only reduces costs, but also reduces the chances of the impending diabetes type 2 epidemic becoming a reality. The skills a patient learns in a Diabetic Prevention Program helps them take care of themselves. Furthermore, reducing specialists, unscheduled appointments, and ER visits for diabetes allows those funds and resources to be reserved until they are needed.
Diabetes diagnoses are often paired with fear. Misunderstandings about the routine maintenance, treatment success rates, and the disease itself can be overwhelming and patients may be treatment hesitant. Providers can ease fear by encouraging a screening in those most at-risk followed by explaining results, answering and addressing patients’ questions and concerns, and letting them know about available care options.
Start the discussion about prediabetes, diabetes, risk factors, and treatments today. Download prediabetes screenings to place in office areas and waiting rooms or share with local community diabetes programs. Learn more about the Midwest Diabetes Conference and watch the recorded webinar on Diabetes Self-Management and Prevention Programs.